Like finely tuned machines, our bodies rely on a balance of chemicals, processes, and reactions to function optimally. One key player in this internal symphony is blood sugar.
But did you know that even if you don’t have diabetes, your blood sugar can sometimes venture into the higher range? This phenomenon, known as non-diabetic hyperglycemia, can be surprising and concerning for many.
Let’s explore the circumstances under which blood sugar might spike even without diabetes. Whether you have a keen interest in health or experience fast glucose spikes, this knowledge can guide better health choices.
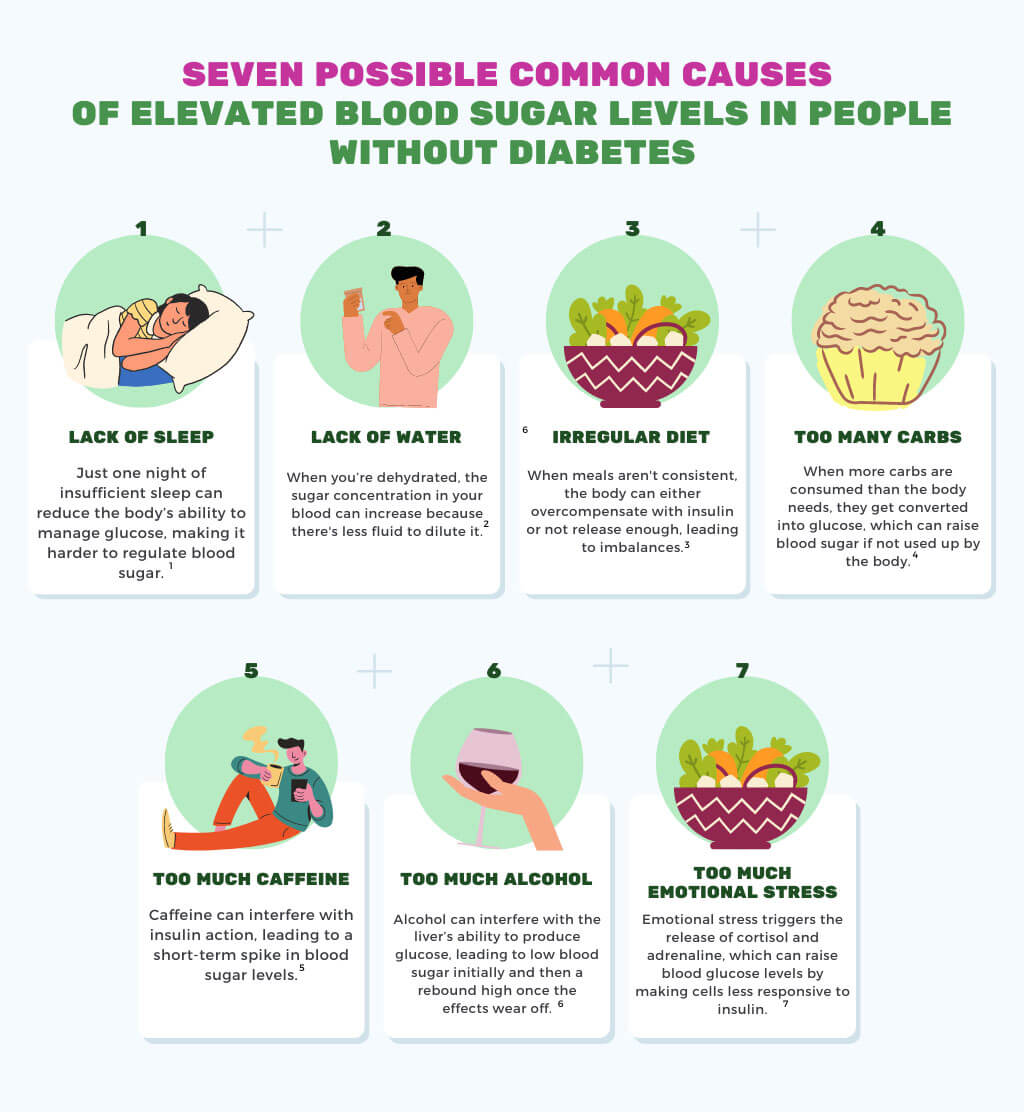
Common Causes of High Blood Sugar in Non-Diabetes
Non-diabetic hyperglycemia is more common than people realize. Diabetes is a significant factor contributing to high blood sugar.
More factors can cause these fluctuations in individuals without diabetes:
- Lack of sleep: Just one night of insufficient sleep can reduce the body’s ability to manage glucose, making it harder to regulate blood sugar; [1]
- Lack of water: When you are dehydrated, the sugar concentration in your blood can increase because there is less fluid to dilute it; [2]
- Irregular diet: when meals aren’t consistent, the body can either overcompensate with insulin or not release enough, leading to imbalances; [3]
- Too many carbs: When more carbs are consumed than the body needs, they get converted into glucose, which can raise blood sugar if not used by the body; [4]
- Too much caffeine: Caffeine can interfere with insulin action, leading to a short-term spike in blood sugar levels; [5]
- Too much alcohol: Alcohol can interfere with the liver’s ability to produce glucose, leading to low blood sugar initially and then a rebound high once the effects wear off; [6]
- Too much emotional stress: Emotional stress triggers the release of cortisol and adrenaline, which can raise blood glucose levels by making cells less responsive to insulin; [7]
Uncommon Causes of High Blood Sugar in Non-Diabetes
Understanding common factors of high blood sugar is crucial, but it’s also important to be aware of less common causes. Sometimes, rare medical conditions or specific events can lead to elevated blood glucose levels, even if you don’t have diabetes. Let’s delve into these uncommon culprits:
Pancreatic Diseases
The pancreas is a vital organ for blood sugar regulation, producing insulin, which helps manage glucose. Diseases affecting the pancreas, such as pancreatitis or pancreatic cancer, can impair its ability to produce insulin. This can lead to elevated blood sugar levels. [8]
Cushing’s Syndromes
Cushing’s syndrome arises when the body produces excessive cortisol, a stress hormone. High cortisol levels can lead to a range of health issues, including elevated blood glucose. This is because cortisol increases glucose production while decreasing insulin sensitivity. [9]
Polycystic Ovarian Syndrome (PCOS)
PCOS, a hormonal disorder common among women of reproductive age, has been linked to insulin resistance. Women with PCOS might experience higher blood glucose levels due to their body’s decreased ability to use insulin effectively. [10]
Infections
While it may seem unrelated, certain infections can cause a temporary spike in blood sugar. This is due to the body’s inflammatory response, which releases stress hormones that impair insulin function. Infections like urinary tract infections or pneumonia can have this effect. [11]
Somogyi Effect
Named after the researcher who discovered it, the Somogyi effect, or “rebound hyperglycemia,” occurs when a significant drop in blood sugar during the night, followed by a rebound effect, causes a surge in blood glucose in the morning. This phenomenon can be triggered by various reasons, such as taking too much insulin or drinking alcohol before going to bed. [12]
A broad understanding of the many factors that influence blood glucose, including the uncommon ones, empowers us to monitor and manage our health. While these conditions are less typical, they highlight the diverse influences on our body’s glucose regulation system.
FAQ
Diving into the intricacies of blood sugar can raise more questions than answers, especially for those newly exploring this topic. Here are some frequently asked questions (FAQ) to provide clarity on common concerns.
Can a cold cause high blood sugar in non-diabetics?
Absolutely! When you’re sick with a cold, your body releases stress hormones to combat the illness. These hormones can lead to increased blood sugar levels. For individuals with diabetes, the effect is more pronounced, but even non-diabetics might observe slight elevations in their blood sugar when battling a cold. It’s the body’s natural response to illness. Ensuring proper hydration, rest, and monitoring blood sugar during diseases is beneficial. [11]
Does vomiting increase blood sugar in non-diabetics?
Vomiting can affect blood sugar levels, though not always directly. When you vomit, you lose fluids and may become dehydrated. Dehydration, in turn, can concentrate the glucose in your blood, leading to higher blood sugar readings. Additionally, vomiting may be a result of an underlying condition or illness, which might raise blood sugar. While an isolated episode might not significantly impact glucose levels, repeated bouts should prompt medical attention and potential blood sugar monitoring. [13]
How to test my blood sugar level at home?
Testing blood sugar at home is straightforward with the help of a blood glucose monitor. Here’s a quick guide:
- Preparation: Start by washing your hands to ensure accuracy. Choose a test strip compatible with your monitor.
- Prick: Using a lancet, gently prick the side of your fingertip. This is usually less sensitive than the pad.
- Test: Place the drop of blood onto the test strip and insert it into the monitor.
- Read: The monitor will display your blood sugar level within a few seconds. Record the reading and the date/time.
- Dispose: Safely discard the used lancet and test strip.
Monitoring your blood sugar at home allows you to understand your body’s reactions to various factors and aids in making informed health choices.
Final Thoughts
Blood sugar management is a universal concern, given the complexities surrounding glucose and the nuances of the human body. Non-diabetic hyperglycemia, although less discussed, highlights that our bodies don’t operate in isolation. Every meal, restless night, or stressful day can influence our internal equilibrium. Common and uncommon triggers demonstrate that many factors can affect our glucose levels, even without the diagnosis of diabetes.
This newfound knowledge is empowering. With the awareness of how diverse elements can impact glucose, we are better equipped to make informed health decisions. It’s not just about managing diagnosed conditions but also about preserving balance and preventing potential future complications.
Technological advancements, like home blood glucose monitors, have further revolutionized our approach. No longer exclusive to diabetics, these tools allow many to gain real-time insights into their body’s reactions, enabling proactive health management. It underscores a shift from merely reacting to health anomalies to actively curating a health-forward life.
In conclusion, our exploration into non-diabetic hyperglycemia is a testament to the body’s intricacies and the interconnectedness of health. As we navigate our daily lives, let’s not just be passive participants but proactive guardians of our health, always ready to learn, adapt, and optimize for well-being.
Resources
- Van Cauter E, Spiegel K, Tasali E, Leproult R. Metabolic consequences of sleep and sleep loss. Sleep Med. 2008;9 Suppl 1(0 1):S23-28. doi:10.1016/S1389-9457(08)70013-3
- Roussel R, Fezeu L, Bouby N, et al. Low water intake and risk for new-onset hyperglycemia. Diabetes Care. 2011;34(12):2551-2554. doi:10.2337/dc11-0652
- Betts JA, Richardson JD, Chowdhury EA, Holman GD, Tsintzas K, Thompson D. The causal role of breakfast in energy balance and health: a randomized controlled trial in lean adults. Am J Clin Nutr. 2014;100(2):539-547. doi:10.3945/ajcn.114.083402
- Augustin LSA, Kendall CWC, Jenkins DJA, et al. Glycemic index, glycemic load and glycemic response: An International Scientific Consensus Summit from the International Carbohydrate Quality Consortium (ICQC). Nutr Metab Cardiovasc Dis. 2015;25(9):795-815. doi:10.1016/j.numecd.2015.05.005
- Lane JD, Barkauskas CE, Surwit RS, Feinglos MN. Caffeine impairs glucose metabolism in type 2 diabetes. Diabetes Care. 2004;27(8):2047-2048. doi:10.2337/diacare.27.8.2047
- Avogaro A, Tiengo A. Alcohol, glucose metabolism and diabetes. Diabetes Metab Rev. 1993;9(2):129-146. doi:10.1002/dmr.5610090205
- Surwit RS, Schneider MS, Feinglos MN. Stress and diabetes mellitus. Diabetes Care. 1992;15(10):1413-1422. doi:10.2337/diacare.15.10.1413
- Karpińska M, Czauderna M. Pancreas—Its Functions, Disorders, and Physiological Impact on the Mammals’ Organism. Front Physiol. 2022;13:807632. doi:10.3389/fphys.2022.807632
- Newell-Price J, Bertagna X, Grossman AB, Nieman LK. Cushing’s syndrome. Lancet. 2006;367(9522):1605-1617. doi:10.1016/S0140-6736(06)68699-6
- March WA, Moore VM, Willson KJ, Phillips DIW, Norman RJ, Davies MJ. The prevalence of polycystic ovary syndrome in a community sample assessed under contrasting diagnostic criteria. Hum Reprod. 2010;25(2):544-551. doi:10.1093/humrep/dep399
- Knapp S. Diabetes and infection: is there a link?–A mini-review. Gerontology. 2013;59(2):99-104. doi:10.1159/000345107
- Monnier L, Colette C, Dunseath GJ, Owens DR. The loss of postprandial glycemic control precedes stepwise deterioration of fasting with worsening diabetes. Diabetes Care. 2007;30(2):263-269. doi:10.2337/dc06-1612
- Hyperglycemia in diabetes – Symptoms & causes – Mayo Clinic. Accessed August 19, 2023. https://www.mayoclinic.org/diseases-conditions/hyperglycemia/symptoms-causes/syc-20373631


