Pregnancy is a remarkable time of growth and change—and part of that involves how your body handles sugar. For some women, this adjustment leads to a condition called gestational diabetes (GDM), which means your blood glucose rises during pregnancy. While the term sounds worrying, the good news is that many cases can be managed well, especially when treated early and with thoughtful lifestyle steps.
This guide is specially tuned for a European audience. We’ll lean on trusted UK-based sources such as National Institute for Health and Care Excellence (NICE) and the National Health Service (NHS) to make sure the advice aligns with clinical practices here. You’ll discover who is more at risk, what to watch out for, and importantly—how to take natural, sensible steps (like your diet and gentle exercise) to steer things in a healthier direction.
Crucially: this is not a substitute for medical care. If you’re pregnant and suspect you may have or are diagnosed with GDM, always keep in close contact with your healthcare team. What we’ll cover here is how to support your body and give yourself the best chance of positive outcomes—alongside, not instead of, professional care.
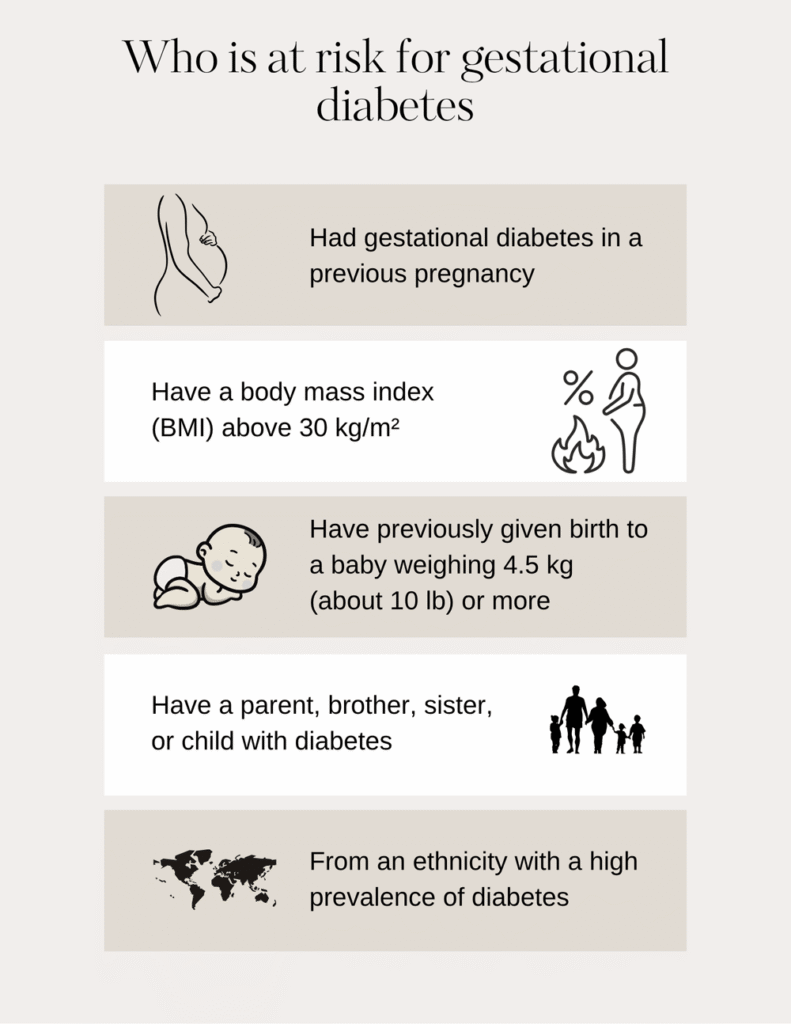
Who is at risk for gestational diabetes?
Gestational diabetes doesn’t happen out of nowhere—some women are simply more likely to develop it because of how their body responds to insulin during pregnancy. According to the National Institute for Health and Care Excellence (NICE, 2020), certain factors increase this risk. Your midwife or doctor will consider these carefully when deciding whether you need an early glucose tolerance test.
You’re more likely to develop gestational diabetes if you:
- Had gestational diabetes in a previous pregnancy
- Have a body mass index (BMI) above 30 kg/m²
- Have previously given birth to a baby weighing 4.5 kg (about 10 lb) or more
- Have a parent, brother, sister, or child with diabetes
- Come from a South Asian, Black, African-Caribbean, or Middle Eastern background (as data show a higher prevalence of GDM in these groups)
If any of these sound familiar, your care team may arrange a 75 g oral glucose tolerance test (OGTT) between 24 and 28 weeks of pregnancy, or sometimes earlier if the risk seems higher. It’s not something you need to self-check at home—your healthcare professionals will guide the testing and interpret the results safely.
Don’t assess by yourself
When you’re expecting, it’s completely natural to want to know everything about your health—and your baby’s. However, when it comes to checking your blood sugar, self-assessment isn’t recommended for diagnosing or predicting gestational diabetes.
According to NICE guidance (NG3, 2020), you should not use tests like fasting plasma glucose, random blood glucose, HbA1c, glucose challenge tests, or even urine dipsticks for sugar to assess your own risk. These tests can be misleading during pregnancy, because your body’s metabolism changes rapidly. Results can vary widely from day to day, and without professional interpretation, they may cause unnecessary worry—or worse, false reassurance.
Instead, the safest and most accurate way to find out is through your antenatal care team. They’ll use proper screening methods, like the oral glucose tolerance test (OGTT), at the right stage of pregnancy. If your results suggest gestational diabetes, they’ll explain what it means and guide you through the next steps for monitoring, diet, and treatment.
In short: stay curious, but don’t self-diagnose. Pregnancy care is a team effort—and your healthcare team is there to keep both you and your baby safe.
Potential dangers of uncontrolled gestational diabetes
Gestational diabetes isn’t something to panic about—but it does need careful management. When blood glucose levels remain too high for too long, it can affect both you and your baby. The goal of monitoring and healthy habits is to keep things in a safe range and prevent these potential complications.
For mums, uncontrolled gestational diabetes can increase the chances of high blood pressure (pre-eclampsia), a condition that may cause complications later in pregnancy. It also raises the likelihood of needing induced labour or a caesarean birth. After delivery, women who had GDM have a higher long-term risk of developing type 2 diabetes—though that risk can often be reduced with lifestyle care after birth.
For babies, consistently high glucose can lead to excessive growth (macrosomia), making delivery more difficult and increasing the chance of birth injury. After birth, some babies may experience low blood sugar (neonatal hypoglycaemia) or mild breathing issues, but these are usually manageable with prompt medical care.
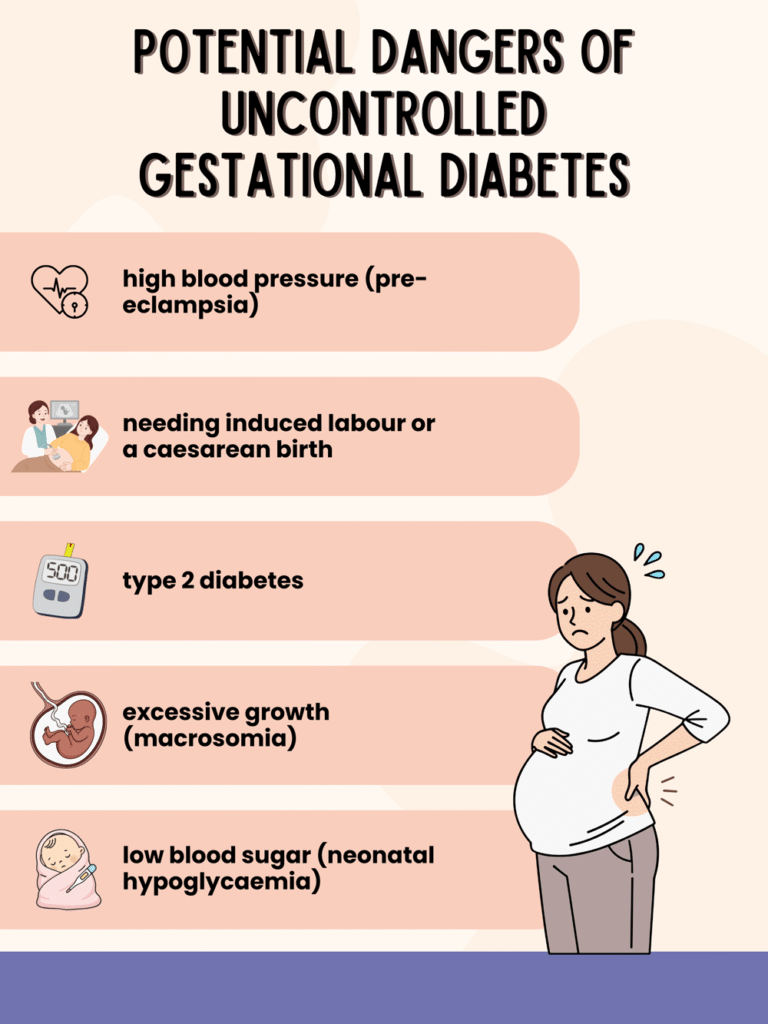
The reassuring part? Most of these risks can be greatly reduced with regular monitoring, a balanced diet, and gentle exercise. When you work closely with your healthcare team, you can help keep your pregnancy safe and healthy—for both of you.
How to manage gestational diabetes naturally
Once you’ve been diagnosed with gestational diabetes, the next question is usually: what can I do about it?
The great news is that many women manage their blood sugar well through simple, consistent lifestyle habits—mainly around food, movement, and monitoring. Let’s start with the first and most powerful part: your diet.
Diet
Pregnancy is not the time for strict dieting—but it is the perfect time for smart, balanced eating. What you eat directly affects your blood glucose levels, so a few steady tweaks can make a real difference.
Don’t skip meals
Skipping meals can cause your blood sugar to drop and then rebound sharply when you finally eat, which puts extra stress on your body. Aim for three balanced meals and two to three healthy snacks per day. Keeping your energy steady helps your baby grow consistently and keeps you feeling more comfortable.
Focus on GI
Choose foods with a low to medium glycaemic index (GI)—they release energy slowly and help prevent glucose spikes. Think wholegrain bread, brown rice, lentils, beans, oats, and non-starchy vegetables. High-GI foods like white bread or sweet cereals can raise your blood sugar too quickly.
More fruit and vegetables
Aim for at least five portions a day, focusing on fresh, frozen, or lightly cooked vegetables. Fruits are healthy too, but go for whole fruit instead of juice and spread them out across the day to avoid sudden sugar jumps.
More protein
Protein helps keep you full and supports your baby’s growth. Include moderate portions of lean meat, fish, eggs, tofu, beans, and dairy. Combining protein with carbohydrates can also help slow sugar absorption.
Less sugary/refined food
Try to reduce foods high in sugar and refined carbs—like biscuits, cakes, pastries, and fizzy drinks. These not only cause glucose spikes but can make you feel more tired afterwards.
Good example: vegan squash and mushroom pie
A hearty, fibre-rich meal like vegan squash and mushroom pie (with wholegrain crust and plenty of vegetables) provides slow energy and great flavour—an ideal dinner choice for balancing blood sugar naturally.
Bad example: biscuits
On the other hand, biscuits or sweet snacks between meals might seem harmless but can quickly raise glucose levels without offering lasting energy. Keep them for rare treats, if at all.

more recipe ideas
Here’s a list of healthy, gestational diabetes–friendly recipes and snack ideas. They are balanced, lower-GI, moderate in sugar, and nutrient-rich.
Breakfast
Overnight oats with chia seeds and berries
- Rolled oats, chia seeds, unsweetened almond milk, and a handful of fresh berries.
- Optional: a sprinkle of cinnamon or a teaspoon of nut butter for extra protein.
Veggie omelette with spinach and mushrooms
- Two eggs, sautéed spinach, mushrooms, and a few cherry tomatoes.
- Serve with a slice of wholegrain toast if you like carbs in the morning.
Greek yogurt parfait
- Unsweetened Greek yogurt layered with flaxseeds, walnuts, and sliced kiwi or berries.

Lunch / Dinner
Vegan squash and mushroom pie
- Use wholegrain crust, plenty of roasted squash, mushrooms, onions, and a chickpea or lentil filling.
Grilled salmon with quinoa and steamed vegetables
- Salmon provides omega-3, quinoa adds protein and slow-release carbs, and lightly steamed veggies keep it fibre-rich.
Chickpea & veggie stir-fry
- Sauté chickpeas, bell peppers, zucchini, and broccoli in olive oil and garlic.
- Serve over brown rice or barley for a lower-GI option.
Lentil & vegetable soup
- Lentils, carrots, celery, onions, and spices.
- Serve with a slice of wholegrain bread for a warming, blood-sugar-friendly meal.

Snacks
- Apple slices with almond butter
- Carrot and cucumber sticks with hummus
- Handful of unsalted nuts (almonds, walnuts, cashews)
- Boiled egg and cherry tomatoes
- Mini wholegrain rice cakes with avocado

Sweet Treat Options (lower sugar)
Chia seed pudding with unsweetened cocoa
Chia seeds soaked overnight in unsweetened almond milk, with a little vanilla extract and cocoa powder.
Baked cinnamon apples
Core an apple, sprinkle with cinnamon, bake until soft. Optional: top with a teaspoon of Greek yogurt.
Energy balls
Mix rolled oats, peanut butter, unsweetened cocoa, and a few chopped nuts. Roll into small balls and refrigerate.

Exercise
Alongside healthy eating, gentle and regular exercise is one of the most effective ways to help control blood sugar during pregnancy. It improves how your body uses insulin and supports steady energy levels throughout the day.
The principle: less intensity, more consistency
You don’t need a tough workout routine—just regular, moderate movement that gets your heart rate up slightly without making you breathless. Think of it as “less intensity, more capacity.” The aim is to move comfortably and often, not to exhaust yourself.
Suitable time: after meal
One of the best times to exercise is 30–60 minutes after eating. Light movement after a meal helps your muscles use up some of the glucose from your food, keeping your blood sugar more stable.
Good example: walking
A simple brisk walk after lunch or dinner can work wonders. Other good options include swimming, prenatal yoga, or stationary cycling—activities that are easy on the joints but still effective.
Stop if not feeling well
Always listen to your body. If you feel dizzy, unusually tired, short of breath, or have pain or cramps, stop immediately and rest. During pregnancy, it’s better to be gentle and consistent than to push too hard.
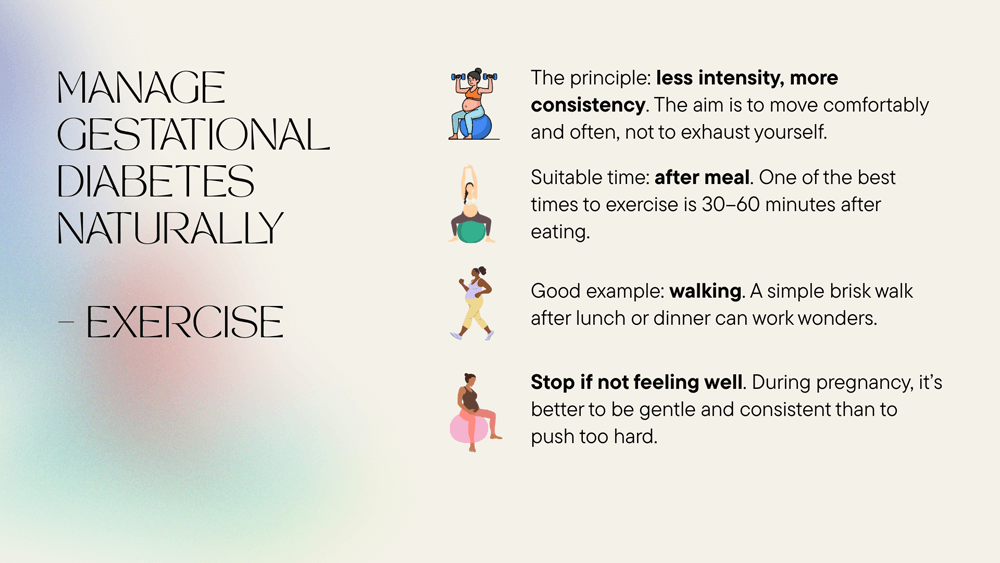
Regular, light exercise—combined with a good diet and medical monitoring—can greatly reduce your need for medication and make you feel stronger and calmer throughout pregnancy.
Monitor
Healthy habits are most effective when combined with regular monitoring. Keeping track of your blood sugar helps ensure your efforts are paying off—and helps your care team adjust your plan if needed.
Routine antenatal care
If you’re diagnosed with gestational diabetes, you’ll receive extra antenatal appointments. During these, your midwife or doctor will:
- Check your blood glucose levels and how well they’re controlled.
- Monitor your baby’s growth and position with ultrasound scans.
- Discuss your diet, activity, and how you’re feeling emotionally.
This care helps ensure both you and your baby stay on a healthy track throughout pregnancy.
Self test
Between appointments, your care team may ask you to check your blood glucose at home, usually with a finger-prick test before and after meals. They’ll provide instructions on how often to test and what your target range should be.
If you find that your healthcare system doesn’t supply enough testing strips or meters, you can consider using a reliable device such as Sinocare’s blood glucose monitor. Consistent self-testing helps you see how different meals or activities affect your glucose levels and keeps you in control of your care.
When to see a doctor
Even if you’re managing your gestational diabetes well through diet and exercise, it’s important to stay in close touch with your healthcare team. Pregnancy can bring rapid changes, and sometimes you’ll need extra support or medical adjustments to keep things on track.
Contact your midwife, GP, or maternity unit as soon as possible if you notice:
- Unusually high or low blood sugar readings despite following your plan
- Blurred vision, excessive thirst, or frequent urination
- Persistent nausea, vomiting, or sudden swelling in your hands, feet, or face
- Reduced baby movement or anything that feels “off” compared with usual
- Signs of infection, such as fever or pain when passing urine
Your doctor might adjust your dietary plan, suggest medication such as metformin or insulin, or arrange more frequent monitoring. Never start or change medicines on your own—gestational diabetes management needs careful supervision to protect both you and your baby.
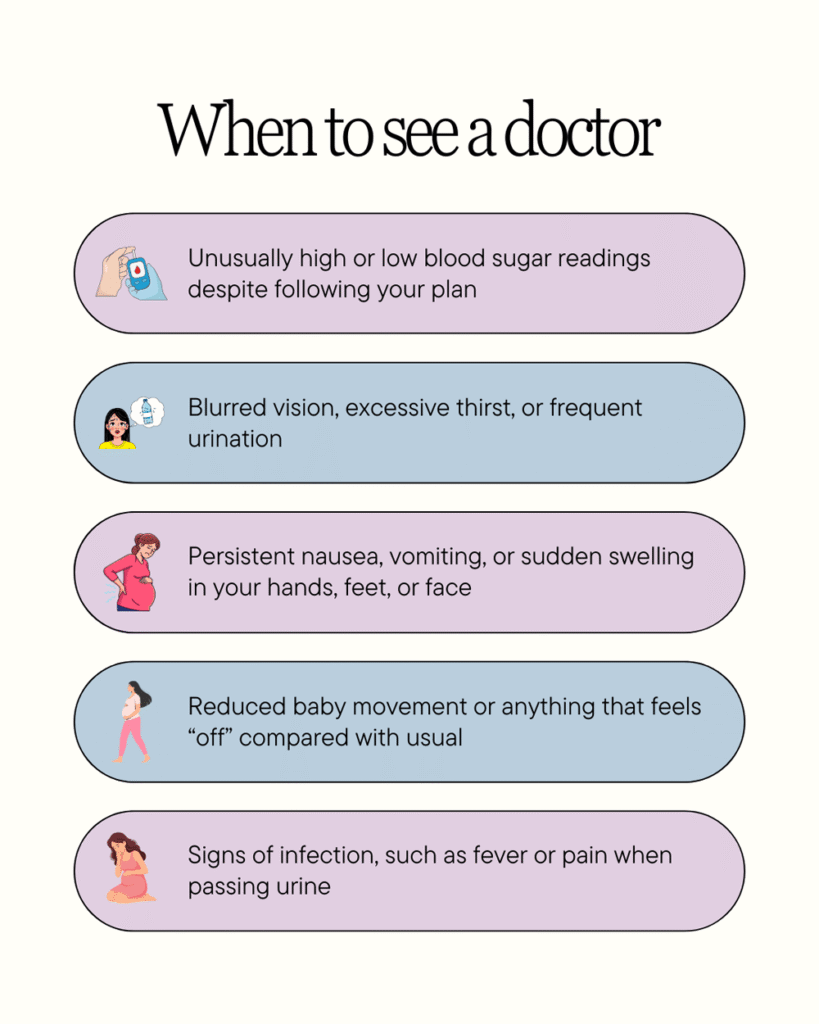
And remember: needing medication doesn’t mean you’ve “failed” natural management. It simply means your body needs a little extra help, and that’s completely normal. The goal is always the same—a safe, healthy pregnancy and a healthy baby.
FAQs
Is gestational diabetes dangerous?
Gestational diabetes can pose risks if it isn’t managed, but with the right care—healthy eating, gentle exercise, and regular monitoring—most women go on to have smooth pregnancies and healthy babies. The key is keeping blood sugar levels within the target range set by your doctor.
Does pregnancy diabetes go away?
Yes, in most cases gestational diabetes goes away after birth. Your healthcare team will usually test your blood sugar levels 6 to 13 weeks postpartum to make sure they’ve returned to normal. However, having GDM once means your lifetime risk of type 2 diabetes is higher, so continuing healthy habits remains important.
What are the symptoms of gestational diabetes?
Many women don’t notice any symptoms at all, which is why screening tests are so important. When symptoms do appear, they might include feeling very thirsty, needing to urinate often, fatigue, or blurred vision—but these can also occur in normal pregnancy, so testing is the only sure way to know.
When do you get tested for gestational diabetes during pregnancy?
If you’re at higher risk, your midwife or GP will arrange a 75 g oral glucose tolerance test (OGTT) between 24 and 28 weeks of pregnancy. In some cases, testing might happen earlier if you have strong risk factors or symptoms.
Is it safe to use Metformin under prescription?
Yes—Metformin is one of the medications considered safe and effective for managing gestational diabetes when diet and exercise aren’t enough. It helps lower blood sugar by improving insulin sensitivity. Always use it under medical supervision, as your doctor will adjust the dose based on your glucose levels and pregnancy stage.
Shall I monitor HbA1c with gestational diabetes?
Generally, no. According to NICE, HbA1c is not used to diagnose or monitor gestational diabetes because pregnancy naturally affects red blood cell turnover. Instead, your daily glucose readings and OGTT results give more accurate insights during pregnancy.
Shall I wear a CGM with gestational diabetes?
Continuous glucose monitors (CGMs) can be helpful for some women, especially if finger-prick tests are difficult or if glucose levels fluctuate a lot. However, not all maternity units provide CGMs for gestational diabetes, and their benefits vary. Discuss with your care team whether this option is suitable for you.
Foods to avoid with gestational diabetes
Try to cut down on foods high in refined sugar and fat, such as cakes, biscuits, white bread, sweetened drinks, and fried snacks. These can cause quick glucose spikes without offering lasting nutrients.
Healthy snacks for gestational diabetes
Opt for snacks that combine protein and fibre, like:
- Greek yogurt with berries
- A handful of unsalted nuts
- Wholegrain crackers with hummus
- Apple slices with peanut butter
- Boiled eggs or cheese sticks
These help keep your blood sugar stable between meals and keep hunger under control.
To wrap up
Managing Gestational Diabetes Mellitus (GDM) doesn’t mean embarking on a radical overhaul—it’s about steady, sensible steps you can keep up. With the right support from your healthcare team, combined with thoughtful diet, gentle activity, and monitoring, you can steer your pregnancy toward a healthy, calm outcome for both you and your baby.
Start with what you can do: eating regularly, choosing slow‑release carbs and protein, getting that post‑meal walk in, and staying mindful of your glucose numbers. Every little habit adds up.
Also remember: having GDM is not your fault and taking medication if needed doesn’t mean you failed. It simply means your body needs a little extra support—just like other parts of pregnancy might (iron, sleep, circulation). With the right approach, most women with GDM go on to have healthy pregnancies and healthy babies.
Stay tuned in to your body, maintain open dialogue with your midwife or doctor, and treat yourself with kindness. You’re doing something incredible. Let’s go healthier—together.
References
- National Institute for Health and Care Excellence. (2020). Diabetes in pregnancy: management from pre‑conception to the post‑natal period (NICE guideline NG3). Retrieved from https://www.nice.org.uk/guidance/ng3
- Royal College of Obstetricians and Gynaecologists. (n.d.). Gestational diabetes. Retrieved from https://www.rcog.org.uk/for‑the‑public/browse‑our‑patient‑information/gestational‑diabetes/
- Titic‑Yulu, I., et al. (2017). Screening of Gestational Diabetes and Its Risk Factors. Journal of Clinical Medicine, 11. https://doi.org/10.3390/jcm11174953
- Minschart, B., et al. (2017). Current guidelines on the management of gestational diabetes mellitus: A narrative review. European Journal of Obstetrics & Gynecology and Reproductive Biology, 207, 205‑213.
- Hod, M., Kapur, A., McIntyre, H. D., et al. (2015). The management of hyperglycaemia in pregnancy: What’s new? Diabetologia, 58(8), 1755‑1769.


